Monkeypox Outbreak: Symptoms, Variants and Trends of the Outbreak, and More
What's happening
The monkeypox outbreak is a global and national public health emergency.
Why it matters
To stop monkeypox from becoming a disease that regularly circulates in the US, we need to slow the outbreak with tools like vaccines and testing.
What it means for you
Anyone can get monkeypox, but men who have sex with men are currently the people most impacted. If you have an unexplained sore or think you may have been exposed, seek medical care and isolate if necessary.
In the US, the number of monkeypox cases has been growing at a slower rate than before, CDC Director Dr. Rochelle Walensky said last week at a press briefing, noting that she's "cautiously optimistic" about some turns the outbreak is taking in the states.
Though many people still need a second dose of the Jynneos vaccine, a new vaccination method is increasing supply. Also, health officials said at the Aug. 26 briefing that gay and bisexual men are taking public health measures that are helping reduce the spread of monkeypox. Men who have sex with men are currently the most impacted in the outbreak, and many have temporarily changed sexual behavior in response to the outbreak in order to minimize risk and transmission of the disease, which is primarily spreading through close and sexual contact.
"The queer community has been central in developing, adapting, and amplifying these messages as the outbreak has unfolded, and the epidemiology further informed our advice to prevent monkeypox," Dr. Demetre Daskalakis, deputy coordinator of the White House National Monkeypox Response Team, said at the briefing.
But despite progress in the monkeypox outbreak response, cases are still being reported, including one death. On Tuesday, Texas health officials reported what appears to be the first death from monkeypox in the US, though officials are still investigating to determine what role monkeypox played in the person's death. More than 18,000 cases of monkeypox have been reported in the US as of Aug. 29, according to data from the US Centers for Disease Control and Prevention.
Though most people will recover at home, monkeypox can be life-threatening for some people, including young children and those with weakened immune systems.
Here's what to know about the disease.

Examples of monkeypox "pox" or rashes.
NHS England High Consequence Infectious Diseases NetworkWhat is monkeypox?
Monkeypox is a disease caused by an orthopoxvirus that belongs to the same family as the viruses that cause smallpox and cowpox. It's endemic in West and Central Africa, and reports of it in the US have been rare but not unheard of. (There were two reported cases in 2021 and 47 cases in 2003 during an outbreak linked to pet prairie dogs.) It's a zoonotic disease, which means it's transmitted from animals to humans.
However, this year monkeypox has rapidly shifted from a regional illness concentrated in African countries to a worldwide outbreak. Because of this, the World Health Organization announced in August that it's changed the names of the two monkeypox variants or "clades." The former Congo Basin/Central Africa clade is now known as Clade I, and the former West African clade is now called Clade II.
Clade II is the one currently circulating worldwide. It has two subvariants, and it's typically less severe than Clade I. The WHO also has said that it's working on finding a new name for monkeypox, which was named before current practices on messaging of viruses and diseases were in place. Those new practices include reducing stigma around a virus.
As of early August, monkeypox is a public health emergency in the US. The declaration was meant to open up more funding and resources needed to respond to the outbreak, including vaccines, testing and treatments. The Biden administration announced the formation of a White House monkeypox response team to advise the administration on how to stop the outbreak.
The federal responses come after criticism over inadequate vaccine access and testing, and a general lack of awareness of the outbreak. The CDC last month announced that the number of tests US labs could run for monkeypox grew from 6,000 to 80,000 specimens per week.
Is there a test? When should I get tested?
The test involves taking a swab from a lesion or sore to test for the virus that causes monkeypox. For people who first develop flulike symptoms before lesions or sores appear, that may mean waiting for lesions or "pox" to appear. If you have symptoms, get tested and isolate at home.
If you were exposed to monkeypox but don't have any symptoms, you don't need to isolate, according to the CDC. But you should continue to monitor yourself for symptoms and take your temperature twice daily, if you can.
The CDC advises reminding your health care provider that monkeypox is circulating. If you think you have monkeypox but are turned down for a test, don't be afraid to seek a second or third opinion to get the care you need. Testing availability is expanding as the outbreak progresses, but because symptoms can vary and monkeypox was previously rare in the US, health providers may initially mistake it for other illnesses.
What are the symptoms of monkeypox?
Symptoms of monkeypox in humans are similar to (but usually significantly milder than) those of smallpox, which the WHO declared eliminated in 1980.
A monkeypox infection can begin with flulike symptoms -- including fatigue, headache, fever and swollen lymph nodes -- followed by a rash, but some people will only develop the rash, according to the CDC. The monkeypox rash or individual sores can look like pimples or blisters and can be found pretty much anywhere on the body, including the hands, genitals, face, chest and inside the mouth or anus. Lesions can be flat or raised, full of clear or yellowish fluid and will eventually dry up and fall off.
You can spread monkeypox until the sores heal and a new layer of skin forms, according to the CDC. Illness typically lasts for two to four weeks. The incubation period ranges from five to 21 days, according to the CDC, which means people will most likely develop symptoms within three weeks of being exposed. For some people, monkeypox lesions can be very painful.
Monkeypox doesn't have the same ability to infect people that the virus that causes COVID-19 has, says Dr. Amesh Adalja, an infectious-disease expert and senior scholar at the Johns Hopkins Center for Health Security. Monkeypox is generally understood to not be contagious during the incubation period (the time between being exposed and symptoms appearing), so it "doesn't have that ability to spread the way certain viruses like flu or SARS-CoV-2 can," Adalja said, referring to the coronavirus.
How do you catch it?
Monkeypox spreads between people primarily through contact with infectious sores, scabs or bodily fluids, according to the CDC, but it can also spread through prolonged face-to-face contact via respiratory droplets, or by touching contaminated clothing or bedding. (Think the close contact you'd have with a sexual partner, the contact you have with strangers dancing at a club, or the contact you have with a household member whom you kiss, hug or share towels with.) Research is underway on whether (or how well) monkeypox can be spread through semen or vaginal fluid.
The "close" in close contact is a key element in the transmission of monkeypox. That, along with the fact that the virus that causes monkeypox appears to have a slower reproduction rate than the COVID-19 virus, sets it apart from the ongoing COVID-19 pandemic, Dr. Tom Inglesby, director of the Center for Health Security at the Johns Hopkins Bloomberg School of Public Health, said in June at a media briefing.
The majority of the cases in the US continue to be in gay and bisexual men, with most of those cases linked to sexual contact. (Monkeypox isn't a sexually transmitted disease, but sexual or intimate contact provides the very close contact monkeypox needs to spread.) Gay and bisexual communities tend to have particularly "high awareness and rapid health-seeking behavior when it comes to their and their communities' sexual health," Dr. Hans Henri P. Kluge, the WHO's regional director for Europe, said in a statement at the end of May, noting that people who sought health care early in the outbreak should be applauded.
Depending on where they live, people at higher risk of catching monkeypox, including men with multiple recent sexual partners, may be able to get a monkeypox vaccine. However, supply has been limited and some people have reported trouble securing an appointment.
Getty ImagesHow severe is monkeypox? Is there treatment?
There are two clades or types of monkeypox virus, according to the WHO: the recently renamed Clade I and Clade II. Clade II, which has been identified in the recent cases, has had a fatality rate of less than 1% in the past. Clade I has a higher mortality rate of up to 10%, according to the WHO.
Though the circulating strain of monkeypox is rarely fatal, according to the CDC, it can be very painful and may result in some scarring. Pregnant people, younger children, people with weakened immune systems and those with a history of eczema may be more likely to get seriously ill.
Antiviral medication like tecovirimat (TPOXX) can be used in people who are at risk of getting severely sick from monkeypox, according to the CDC. This treatment isn't approved specifically for monkeypox (it's meant for treating smallpox) and access to it has been restricted, with paperwork and strict ordering instructions. However, the CDC recently loosened restrictions around the drug. On Aug. 26, health officials said TPOXX should be even more available now and that there's "three times as many treatment courses as there are monkeypox cases."

Monkeypox lesions progress through a series of stages before scabbing, according to the CDC. Though traditionally the rash starts on the face before becoming more widespread, monkeypox blemishes can be limited, resemble a pimple or other sore and aren't always necessarily accompanied by flulike symptoms.
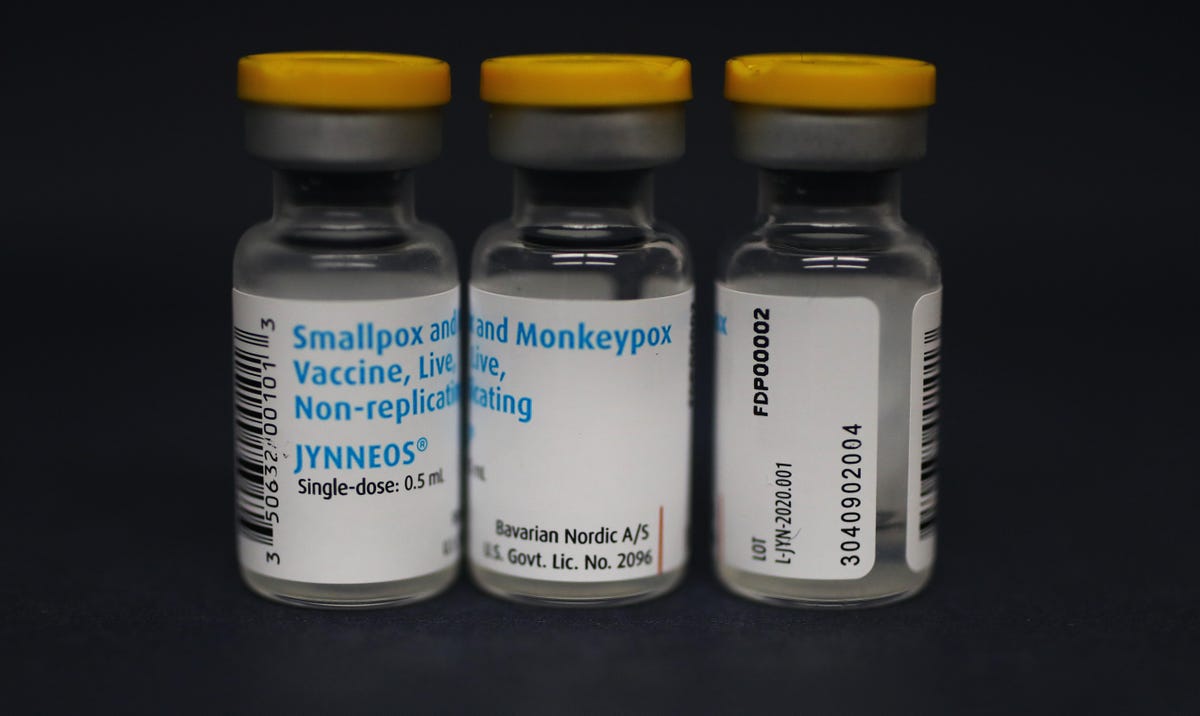
Getty Images/HandoutIs there a vaccine?
Yes. The US Food and Drug Administration has approved Jynneos to prevent smallpox and monkeypox. Because monkeypox is so closely related to smallpox, vaccines for smallpox are also effective against monkeypox. In addition to Jynneos, the US has another smallpox vaccine in its stockpile, called ACAM2000. Because ACAM2000 is an older generation of vaccine with harsher side effects, it's not recommended for everyone, including people who are pregnant or immunocompromised.
Jynneos is the vaccine currently available to people who are at higher risk of getting monkeypox, or may have already been exposed to it. The FDA recently authorized a new way of giving people Jynneos that will stretch out the limited supply through intradermal vaccination, which requires a lower dose of vaccine compared to subcutaneous injection. (Basically, now people will get the vaccine under a top layer of skin as opposed to the standard shot that goes right into the arm.)
Vaccinating people who've been exposed to monkeypox is what Adalja calls "ring vaccination," where health officials isolate the infected person and vaccinate their close contacts to stop the spread. But vaccinating people with a confirmed exposure, in addition to people at risk of being exposed in the near future, may be crucial to getting control of the outbreak, according to the White House's chief medical adviser, Dr. Anthony Fauci.
Dr. Daniel Pastula, chief of neuroinfectious diseases and associate professor of neurology, medicine and epidemiology at the University of Colorado Anschutz Medical Campus, said the vaccine is used in people who've been exposed but aren't yet showing symptoms of monkeypox, because the incubation period for the disease is so long.
"Basically what you're doing is stimulating the immune system with the vaccine, and getting the immune system to recognize the virus before the virus has a chance to ramp up," Pastula said.
Though health care and lab professionals who work directly with monkeypox are recommended to receive smallpox vaccines (and even boosters), the original smallpox vaccines aren't available to the general public and haven't been widely administered in the US since the early 1970s. Because of this, any spillover or "cross-protective" immunity from smallpox vaccines would be limited to older people, the WHO said.
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.
Source
Tags:
- Monkeypox Outbreak Symptoms Variants And Trends Of Electronegativity
- Monkeypox Outbreak Symptoms Variants And Trends Of Today
- Monkeypox Outbreak Symptoms Variants And Trends Magazine
- Monkeypox Outbreak Symptoms Variants And Vaccines
- Monkeypox Outbreak Symptoms Variants And Pfizer
- Monkeypox Outbreak Symptoms Variants Meaning
- Monkeypox Outbreak Symptoms Variants Synonym
- Monkeypox Outbreak 2022 Update
- Monkeypox Outbreak Map
- Human Monkeypox Outbreak
Blog Archive
-
▼
2023
(199)
-
▼
January
(84)
- Logan Paul Has Just Signed With The WWE
- Heat Pump Vs. Furnace: Learn The Difference Betwee...
- Soon You'll Be Able To Book Office Spaces Through ...
- How To Fix 5 Common Causes For Your Home Internet ...
- Polar Pro Venture3+ Lens, Filter Pack Helps You Ge...
- Find Out What's Coming In The Mail Before It's Del...
- This 43-Inch Amazon Fire TV Is Down To Its Lowest ...
- Save Up To $250 On A Premium Samsung Tablet Today ...
- Wordle: What To Know About The Viral Word Game
- Gaming Monitors From CES 2022 To Get Hyped For
- 2023 Honda CR-V Teased Ahead Of Summer Debut
- James Webb Space Telescope's Smooth Launch Extende...
- Save Big On Motorola Phones With Prices Starting A...
- Ouya Teams With Xiaomi To Bring Video Games To China
- The Best Cat Toys, According To Our Favorite Felines
- Nvidia To Buy SoftBank's Arm Chip Division For $40...
- 5 Great Last-minute Gifts To Make With Your 3D Pri...
- GM Announces Plans For National EV Fast Charging N...
- 2022 Kia Sorento Receives Price Hikes Across The B...
- T-Mobile Is Offering Unlimited Google Photos Storage
- Amazon To Acquire One Medical In Major Boost To It...
- Lenovo Glasses T1 Are Wearable Displays That Also ...
- 'MythBusters' Adam Savage Tests DJI Inspire 1 4K Q...
- Best Home Security Deals For Black Friday: Save On...
- TikTok Live To Feature Hour-Long Sketch Comedy Sho...
- Air Frying Vs. Baking: What's The Best Cooking Met...
- Crocheted Predator Costume Goes On The Hunt For Ha...
- Acer Goes After The Classroom With New Durable Spi...
- Google Store Stumbles During Pixel 6 Phone Launch
- WhatsApp Will Let You Move Chat History Between IO...
- Monitor OS X LaunchAgents Folders To Help Prevent ...
- Motorola Edge Plus 2022 Vs. 2020: It's Not An Easy...
- GoPro, Red Bull Partner To Capture The World Of Ex...
- Facebook's $37.5 Million Location Tracking Settlem...
- Apple Rumored To Be Working On A Foldable IPad/Mac...
- Asus ROG Phone 6, 6 Pro Gaming Phones Bring Samsun...
- Nintendo Of America Testers Allege Sexual Harassme...
- Kia EV9 Electric Concept Previews A 3-row Producti...
- These Stunning Pens Bring Back The Joy Of Writing
- 7 Ways To Save Money On Car Insurance
- Best Immersion Blender For 2022
- The IPhone At 15: How Apple's Phone Became The Cen...
- TikTok's China Equivalent Limits Kids To 40 Minute...
- You Can Now Play Wordle On NYT Crossword App
- How To Remove Wallpaper In An Old Or Period House
- 60 Super-cool Kitchen Gadgets You Can Get For Less...
- Apple's 16-inch MacBook Pro Gets Graphics Boost Wi...
- MLB TV Review: Subscribers May Balk At Increased B...
- Monkeypox Outbreak: Symptoms, Variants And Trends ...
- Samsung Galaxy S22 Ultra Vs. Pixel 6 Pro: It's A T...
- Asus ZenBook Duo 14 UX482 Review: A Dual-screen La...
- Leaked Pics Of Huawei's Updated Freebuds Show Wire...
- Samsung QN90B QLED Vs. LG C2 OLED: Which TV Is Bes...
- Don't Swap Your Gas-Guzzler For An Electric Vehicl...
- 6 Important Things To Know About Your Social Secur...
- Universe's Most Massive Known Star Imaged With Unp...
- Xiaomi Mi Smart Projector 2: High Style, Low Brigh...
- Asus ZenBook 13 UX333 Review: New Asus ZenBooks Pa...
- WWE Hell In A Cell 2020: Results, Full Recap And N...
- Red Alert! New Honda Civic Type R Coming Next Year...
- Meta Has A Giant New AI Supercomputer To Shape The...
- 2022 Kia EV6 Review: Best Foot Forward
- Shop Coach Outlet's Varsity Collection With Prices...
- Pixar's 'Turning Red' Teams Up With Firefox To Cel...
- Shopping At Wayfair? These 3 Simple Tips Will Make...
- Facebook Is Growing Its Daily Users Again
- Moto G Fast Vs. G Power Vs. G Stylus: Motorola Bud...
- WWE Elimination Chamber 2022: Start Times, Full Ca...
- The IPhone SE, Not The Mini, May Be The Future Of ...
- RedMagic 7S Pro's Highlight Feature May Be Its Hid...
- 2021 Honda Accord Reveal: Fresh Style, More Tech B...
- Motorola Edge Plus Hands-on: A $1,000 5G Phone Wit...
- Best High-Tech Ski Gear For 2022
- Google In Hot Water For Sending Unwanted Ad Emails
- Hisense Recalls French-Door Fridge Due To Injury R...
- The App That Helps Prepare You For Death
- Your MacBook Trackpad Has An Annoying Setting You ...
- Acer Chromebook R11 Review: A Finger-friendly Hybr...
- The IPhone At 15: Steve Jobs Revealed His Greatest...
- Universe's Most Massive Known Star Imaged With Unp...
- Bored Kids? Get Them This Indoor Beginner Drone Fo...
- Thirsty Suitors: Battle Your Exes In This Colorful...
- HP's New Spectre Laptops Have A Webcam Kill Switch...
- Are USDA Loans Available To Everyone? How To Know ...
-
▼
January
(84)
Total Pageviews
Search This Blog
Popular Posts
-
Contoh soalan fizik spm 2019, contoh soalan fizik spm 2018, contoh soalan fizik spm 2017, contoh soalan fizik kertas 3, contoh soalan fizik ...
-
Ukuran tv, ukuran tv 32 inch, ukuran tv 40 inch, ukuran tv 42 inch, ukuran tv 60 inch, ukuran tv 42, ukuran tv lcd, ukuran tv led, ukuran tv...
-
Ukuran sepatu, ukuran sepatu us, ukuran sepatu anak, ukuran sepatu eu, ukuran sepatu eur, ukuran sepatu nike, ukuran sepatu adidas, ukuran s...
